Tricuspid Atresia
What is tricuspid atresia?
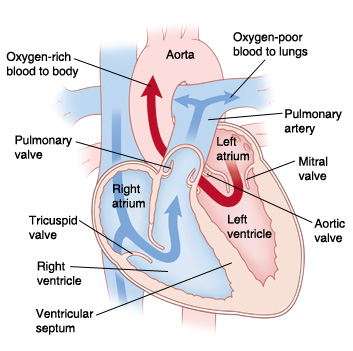
Tricuspid atresia (TA) is a heart defect present at birth (congenital). It occurs when the tricuspid valve doesn’t form, or only partly forms. Normally the tricuspid valve is located between the right upper chamber (atrium) and the right lower chamber (ventricle) of the heart. Instead of a valve, a piece of tissue forms that restricts blood flow between the right atrium and right ventricle. The defect keeps low oxygenated blood from flowing normally into the right atrium to the right ventricle, and to the lungs where the blood becomes oxygenated. With TA, there is mixing of low oxygenated blood with oxygenated blood. This means not enough oxygen in the blood is carried to the body. This may cause a blue coloring of the skin or lips.
In tricuspid atresia, the following occurs:
The tricuspid valve doesn't form correctly or at all.
The right ventricle is often smaller than normal.
There is an opening between the two atria (atrial septal defect). This is often an open (patent) foramen ovale. The foramen ovale is a normal part of fetal circulation that usually closes shortly after birth.
There is an opening between the ventricles (ventricular septal defect).
An open (patent) ductus arteriosus lets blood flow from the aorta to the pulmonary artery. This lets blood flow to the lungs for oxygen. The ductus arteriosus is a normal part of fetal circulation. It usually closes shortly after birth.
Other heart defects may also be present. These may include transposition of the great vessels, pulmonary stenosis, or pulmonary atresia.

What causes tricuspid atresia?
A baby's heart develops during the first 8 weeks of pregnancy. In TA, the tricuspid valve doesn't form as it should. Development of the ventricles is helped by blood flowing through them. Because blood doesn't pass through the tricuspid valve, the right ventricle remains small.
Some congenital heart defects may be passed down through families (genetic defects). Most of the time, there is no known cause for TA.
What are the symptoms of tricuspid atresia?
Symptoms of TA occur shortly after birth. Common symptoms may include:
Blue color of the skin, lips, and nail beds (cyanosis)
Fast breathing
Trouble breathing
Fast heart rate
Poor feeding
The symptoms of TA may look like other health conditions. Have your child see their healthcare provider for a diagnosis.
How is tricuspid atresia diagnosed?
TA may be diagnosed with a prenatal ultrasound exam. Otherwise, symptoms occur shortly after birth. A pediatric cardiologist or a neonatologist will help care for your child. These are healthcare providers with special training to treat problems in children.
One or more healthcare providers will examine your baby. They will listen to your baby's heart and lungs with a stethoscope and note any abnormal heart sound (heart murmur).
Testing for congenital heart disease may include:
Pulse oximetry. A simple test that uses a small probe to check the amount of oxygen in the blood.
Lab tests. Blood and urine samples will be checked.
Chest X-ray. A chest X-ray may show changes often seen with TA.
Electrocardiogram (ECG). An ECG records the electrical activity of the heart. It shows abnormal rhythms and finds heart muscle stress.
Echocardiogram (echo). An echo uses sound waves to make a moving picture of the heart and heart valves. The diagnosis of TA will be made based on finding the abnormal heart structures.
Heart cath (cardiac catheterization). This procedure gives very detailed information about the structures inside the heart. Your child will be given medicine to relax (sedation). Then a thin, flexible tube (catheter) is put into a blood vessel in your child's groin. Under continuous X-ray (or fluoroscopy), the catheter is guided to the heart. Blood pressure and oxygen measurements are taken in the heart chambers, the pulmonary artery, and the aorta. Contrast dye is also injected to more clearly see the structures inside the heart. A heart cath is not often done to diagnose this condition. But it may be done before surgery and in the early treatment of the defect.
How is tricuspid atresia treated?
Your child will most likely be in the intensive care unit (ICU). Early medical treatment may include:
Supplemental oxygen or possibly a mechanical breathing machine (ventilator) to help with breathing
Medicines may be given to help the heart and lungs work better. Prostaglandin E1 may be given to keep the ductus arteriosus open.
Other early treatment may include:
Cardiac cath. In some cases, cardiac cath may be used in the early period. If pulmonary stenosis is present, a catheter with a balloon at the tip can be inflated to widen the valve and let enough blood flow through.
Balloon atrial septostomy. A special catheter with a balloon in the tip is used to create or enlarge an opening in the wall between the left and right atria (atrial septum). This helps with blood flow from the right side of the heart to the left side of the heart.
Three surgeries, in stages, may be done. They include:
Blalock-Taussig shunt. This surgery is done on newborns. It varies, depending on the exact defect your child has. A connection (shunt) is created to let blood from the aorta reach the lungs and pick up oxygen.
Glenn shunt. This surgery may be done on babies ages 2 to 6 months. A new connection (shunt) replaces the first shunt. This shunt connects the large blood vessel from the top of the body to the heart (superior vena cava) to the pulmonary artery. This allows blood to get to the lungs for oxygen.
Fontan procedure. This surgery may be done from ages 2 to 3. A second connection (shunt) is made. It allows blood from the large blood vessel from the lower part of the body to the heart to flow to the pulmonary artery. This surgery varies depending on the exact defect, as well as other factors.
What are possible complications of tricuspid atresia?
Complications of TA may include:
Not enough oxygen getting to the body's tissues (hypoxemia)
Enlarged right atrium
Heart rhythm problems (arrhythmias)
Less ability to exercise
Heart failure
Poor growth and development
Death
Living with tricuspid atresia
Your child may need a series of repair procedures.
Before your child comes home, the nursing staff will explain medicines and treatments. For instance, your child may need special formula and supplemental feedings to help them grow. The staff will also help to arrange home healthcare, if needed. You may get other instructions from your child's heart care team and the hospital staff.
Babies will have a blue color to their skin (cyanosis) after the first two surgeries, or until the final Fontan procedure is done. Your child may grow and develop slowly because of decreased oxygen in the blood. After the Fontan procedure, when oxygen levels get better, you will likely see large improvements in your child's growth and development.
Your child will need to be seen often by a pediatric cardiologist. The cardiologist may advise:
Your child should get all advised vaccines.
Your child will likely need antibiotics before some types of surgery or dental procedures.
Your child may not be able to take part in some sports.
As your child grows and matures, they will need to work with a cardiologist and other healthcare providers to plan pregnancy or surgeries.
Regular follow-up care at a center offering pediatric or adult congenital cardiac care should continue throughout life.
Talk with your child's cardiologist about the specific outlook for your child.
When should I call my child's healthcare provider?
Call your child's healthcare provider if your child's normal symptoms become worse or if new symptoms appear.
Key points about tricuspid atresia
Tricuspid atresia (TA) occurs when the tricuspid valve does not develop correctly. This prevents blood flow from the right atrium to the right ventricle.
TA may be identified during a prenatal ultrasound or shortly after birth when the baby has symptoms like turning blue (cyanotic).
Your child will stay in the intensive care unit (ICU).
Your child will need medicines and a series of surgeries to allow oxygen-rich (red) blood to be pumped to the body.
Your child will need to be followed by a specialist in congenital heart conditions throughout their life.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
Know the reason for the visit and what you want to happen.
Before your visit, write down questions you want answered.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your healthcare provider gives you for your child.
Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
Ask if your child’s condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if your child does not take the medicine or have the test or procedure.
If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your child’s healthcare provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Connect with us:
Download our App: